PG17. Female Genital Mutilation (FGM)
For a record of all amendments and updates, see the Amendments & Archives.
Specific definitions of key concepts used by safeguarding practitioners are available through the Glossary.
AMENDMENT
In April 2024 information was added about NHS data sharing – this is a national IT system that supports the early intervention and ongoing safeguarding of girls, under the age of 18, who have a family history of Female Genital Mutilation.
"I hope I'll be alive to see that day when we don't have FGM anymore….I broke the chain in my family, and I can't wait for the day when we see that chain break for good."
Hibo Wardere, anti-FGM campaigner1. Introduction
Female genital mutilation is child abuse and constitutes significant harm. Child protection procedures should be followed when there are concerns that a girl is at risk of, or is already the victim of, FGM.
This procedure summaries the responsibility of professionals and volunteers to intervene effectively to prevent the genital mutilation of girls and to support those who have been the victim of FGM. For many professionals and volunteers this will mean being aware of which girls are at risk of, or may have already experienced, FGM and knowing how to report these concerns. For others who have more specific safeguarding responsibilities, it will involve complex work to safeguard girls, support victims and prosecute perpetrators. For everyone, it will involve questioning attitudes and beliefs that may get in the way of identifying girls who are at risk of FGM and which may also get in the way of providing the consistent, determined support these girls need to keep them safe.
For more details please refer to the 'Multi agency statutory guidance on female genital mutilation'.
Significant change is required as existing practice has identified very few victims and has failed to prosecute any offenders despite the fact that FGM has been illegal in the UK since 1985. Low rates of identification of FGM should not be taken to mean that the number of girls who've experienced FGM, or are at risk of FGM, is small. A recent report [1] has estimated that nearly 10,000 girls age 0-14, born in FGM practising countries and now living in England and Wales, will have either undergone FGM prior to migration or are likely to undergo FGM as they grow to adulthood. In addition to these girls, between 1996 and 2010, 144,000 girls were born in England and Wales to mothers from FGM practicing countries and it is estimated that 60,000 of these girls [2] were born to mothers with FGM.
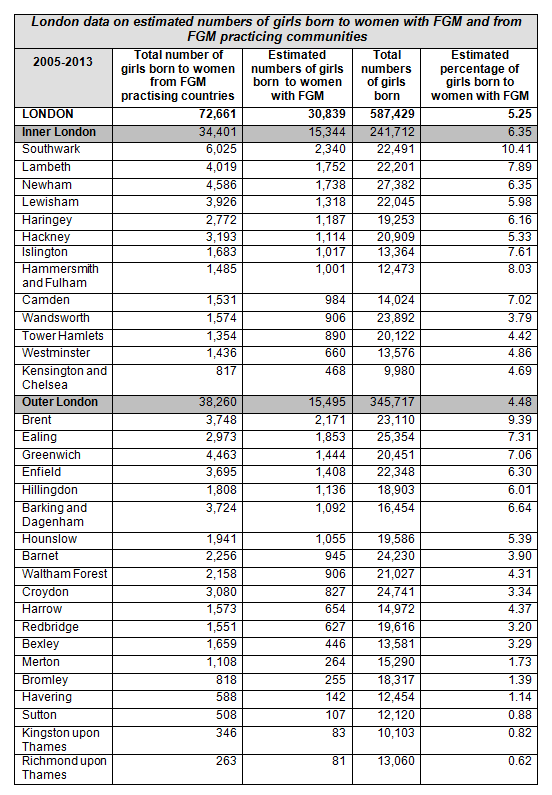
The estimated number of girls born to mothers who have had FGM varies considerably but London has by far the largest percentage. Within London, Southwark, at 10.41%, has the highest estimated percentage - this would equate to 2,340 girls born between 2005 and 2013. Brent has the second highest estimated prevalence at 9.39% and this would equate to 2,171 girls born in the same time period. See section on prevalence below for all London Local Authority data.
It should be noted that whilst the impact of migration on the prevalence of FGM is not known and the above figures are based on estimated risk in country of origin, even if, as a result of migration only 25% of girls born to mother with FGM experienced FGM themselves, it would still mean that between 2005 and 2013 over 7000 girls in London would have experienced FGM or would do so before they reached adulthood.
[1] www.city.ac.uk/news/2015/july/no-local-authority-area-in-england-and-wales-free-from-fgm
[2] Defined as girls aged between 0 and 14 in 2011
A Lifelong Trauma
There's no excuse for cutting children's bits off in the name of culture or religion. There's absolutely no reason that should ever happen. We need to get the cultural thing completely out the way. It's child abuse full stop[3].
Ayshah, who was cut at age 5 in Somalia
FGM is a terrible crime with life-long consequences for the girls who suffer it. Survivors talk eloquently of the horror of their experiences and the impact it has had on their lives and it is with their stories that this guidance starts:
Hibo Wardere, an anti-FGM campaigner who was forced to get cut aged six in Somalia, talked about her experience in an interview:
She describes the ordeal as "being engulfed in pain from head to toe – like fireworks going off everywhere and you don't know how to stop them. I prayed to God to just take me then and there. The emotional impact it had on me was huge – I couldn't look at my mum anymore," she remembers. "All I could see was my hatred and my despair." Every day for the next 10 years, she would ask her mother why she had been subjected to such brutality.
She experienced Type III FGM and goes on to say:
"I used to think marriage was horrible because every female relative I had would end up in hospital after getting wed," she says. "I made my cousin promise to tell us what happened and, one month after her wedding, she came back looking gaunt and unhappy. She told us, 'remember how we got cut when we were little? Your husband has to bulldoze that.'" As the girl lay in a pool of blood in her marital bed, her family danced around, elated that she had been proved a virgin. It was only later that she was taken to hospital for treatment[4].
Kezia Bianca, an anti-FGM campaigner who was cut age 15 in Kenya, describes her experience:
Still from the background I could hear the women singing and I felt that they were celebrating my pain, but the real reason for the songs was to diffuse the cries so that nobody can hear me crying. Then I felt a very sharp pain between my legs. This was a turning point in my life. The pain I felt can't be described; thinking of it brings cold shivers inside me. I was circumcised, I felt incomplete and completely out of control…At the back of my mind so many questions were going through my head: what will happen after this? Will this pain ever leave my life? Will I be able to walk again in my life? … My life took a complete turn, I felt wasted and hopeless – the rest is history[5].
Hodda, an FGM victim, age 23, and a British resident:
Hodda had type 3 FGM when she was a child. After she was cut, she was sewn back up with and left with a hole no bigger than matchstick that has left her with a host of health problems - and infertile. She said: 'I was seven when I was cut. I remember everything. It happened, I was cut and I got this pain every night, abdominal pain.'[6]
Survivors talk of the agony they experienced when the mutilation took place, the feeling of being out of control and of the sense of betrayal that lasts a lifetime. They describe flashbacks in later life and the harm that can continue into marriage when sex can be a painful and traumatic experience.
[3] www.bbc.co.uk/newsbeat/article/31094612/we-wanted-to-be-cut-says-female-genital-mutilation-survivor
[4] www.telegraph.co.uk/women/womens-life/11390949/FGM-survivor-The-pain-was-so-bad-I-prayed-to-God-to-take-me-then-and-there.html
[5] womenleadingchange.wordpress.com/2012/05/23/female-genital-mutilation-my-story/
[6] Read more: www.dailymail.co.uk/femail/article-2989409/Victims-female-genital-mutilation-speak-s-revealed-thousands-Brits-planning-cut-daughters.html#ixzz3iQnsMJuT
A Hidden Crime
FGM has been a hidden crime in part because there is a culture of silence within practicing communities and because, for the girls who are victims, telling people involves telling on their parents. It is also the case that anyone who speaks out may fear being targeted by those in the community who want to continue the practice. This is why the Serious Crime Act 2015 introduced life-long anonymity for victims of FGM - see section on Legislation and Statutory Guidance below.
The lack of progress in identifying victims and prosecuting perpetrators may also, in part, be the result of ambivalent attitudes towards female sexuality and the importance of female sexual pleasure within British culture. For example, much of the information [leaflets/ posters etc.] about FGM emphasise problems during childbirth and with menstruation and urinary tract infections and does not address the impact of FGM on women's enjoyment of sex.
There is also concern that FGM has not been effectively addressed because of misplaced concerns regarding cultural sensitivity.
Hard facts about how many girls are being cut, where and by whom, are scarce because, according to campaigners, the issue has been neglected by successive governments scared of confronting so-called cultural practices [7].
For all these reasons and more, girls who've experienced FGM are not getting the support and medical assistance they require to recover, perpetrators are not being prosecuted and those girls at risk of FGM are not being identified and protected.
[7] www.theguardian.com/society/2014/feb/06/female-genital-mutilation-foreign-crime-common-uk
2. Definition
Female genital mutilation (FGM) comprises all procedures that involve partial or total removal of the external female genitalia, or other injury to the female genital organs for non-medical reasons. It is important to note that the procedure has no health benefits.
FGM has been classified by the World Health Organisation (WHO) into four types:
- Type 1 – Clitoridectomy: partial or total removal of the clitoris (a small, sensitive and erectile part of the female genitals) and, in very rare cases, only the prepuce (the fold of skin surrounding the clitoris);
- Type 2 – Excision: partial or total removal of the clitoris and the labia minora, with or without excision of the labia majora (the labia are the 'lips' that surround the vagina);
- Type 3 – Infibulation: narrowing of the vaginal opening through the creation of a covering seal. The seal is formed by cutting and repositioning the inner, or outer, labia, with or without removal of the clitoris; and
- Type 4 – Other: all other harmful procedures to the female genitalia for non-medical purposes, e.g. pricking, piercing, incising, scraping and cauterising the genital area.
For more detail, please refer to the Multi–agency Statutory Guidance on Female Genital Mutilation (April 2016).
Click here to access the GOV.UK website for Female Genital Mutilation.
3. The Rights of Girls and Women
FGM is an inhuman act which affects a girl's biological make-up. As a girl I strongly believe that I have the responsibility to protect young girls from this act….Women and men should be made aware of the fact that living free of violence is a basic human right. Also, well-meaning parents who view FGM as a way to prepare daughters for marriage should change their behaviour and recognize that the practice is a violation of the rights of girls [8]. (Kezia Bianca)
FGM is recognized internationally as a violation of the human rights of girls and women. It reflects deep-rooted inequality between the sexes, and constitutes an extreme form of discrimination against women.
- More than 125 million girls and women alive today have been cut in the 29 countries in Africa and Middle East where FGM is concentrated;
- FGM is mostly carried out on young girls sometime between infancy and age 15 and is a violation of the rights of children;
- The practice also violates a girl's rights to health, security and physical integrity, the right to be free from torture and cruel, inhuman or degrading treatment, and the right to life when the procedure results in death.
The practice is mostly carried out by traditional circumcisers, who often play other central roles in communities, such as attending childbirths. However, more than 18% of all FGM is performed by health care providers, and the trend towards medicalisation is increasing [9].
[8] womenleadingchange.wordpress.com/2012/05/23/female-genital-mutilation-my-story/
[9] www.who.int/mediacentre/factsheets/fs241/en/
Why is it carried out?
FGM is carried out in order to reduce the possibility that the girl/woman will enjoy sex and, depending on the type of FGM practised, make sex painful and psychologically traumatic. By making sex unpleasurable and/or painful, girls are mutilated in order to reduce their desire to have sex and hence to try and ensure that they will be a virgin before marriage and sexually faithful during marriage [10].
The control of female sexuality has been linked to family and community honour. Where the strict control of female sexuality is integral to the maintenance of family honour, parents may believe they are carrying out FGM for the long term benefit of their community, family and also their daughters.
FGM is a social and cultural norm for practicing communities, and hence is also carried out to ensure conformity to societal expectations.
Hibo Wardere writes of a conversation she had with her mother as her mother lay on her deathbed: "One night, my mum came out of nowhere and said: 'I need you to forgive me for what I did.' I told her that I already had, years ago." But the moment of reconciliation soured when Wardere explained that she would never allow her own girls to be put through the same torment. "Her face dropped with shock, and there was sadness in her eyes" she remembers. "I felt angry afterwards. I'd just explained why I'd forgiven her but she still thought, on her deathbed, that I should circumcise my girls [11].
Breaking with powerfully held social norms can be very frightening and can lead to ostracisation and to girls being considered 'unmarriageable'. It can also be dangerous and lead to repercussions not only for the individual girl but also her family and wider social network.
Religion and FGM
In communities where FGM is a social norm, it is practised by Muslims, Christians and followers of indigenous religions which suggests that the practice is more cultural than a religious practice [12]. Some Muslim populations believe it to be a religious requirement to practise FGM although FGM is not mentioned in the Koran, the practice of FGM predates Islam and most Muslims in the world do not know about FGM [13].
[10] Attempts to control and limit women's sexual desires cross cultures and religions. For example in Victorian England, FGM was advocated by medical professionals when a girl or young woman was thought to be masturbating.
[11] www.telegraph.co.uk/women/womens-life/11390949/FGM-survivor-The-pain-was-so-bad-I-prayed-to-God-to-take-me-then-and-there.html
[12] National FGM Centre
[13] www.religioustolerance.org/fem_cirm.htm This site presents a number of papers discussing the practice of FGM by Islamic scholars and Muslim women.
4. The Sexual, Physical and Emotional Harm caused by FGM
It is often emphasised that FGM is a one-off act, however, FGM is never a one-off event. It has life-long sexual, physical and psychological consequences for the girls who experience it and is carried out because of powerfully held beliefs about the need to control female sexuality - these beliefs are also likely to impact on a girl if she goes on to deviate from the expected sexual behaviour. For example, she has, or is thought to have, boyfriends or girlfriends prior to marriage.
Sexual Harm
FGM inhibits the ability of girls and women to experience pleasurable sexual sensation and to achieve orgasm. In addition, many girls and women will find sex psychologically painful and sexual intercourse physically painful and may experience sexual phobia.
Physical Harm
When the procedure is carried out, the baby or girl will normally experience pain, and, as the procedure is often carried out without anaesthetic, this pain will often be extreme.
FGM can be fatal with babies /girls dying from blood loss or infection. It can also cause severe bleeding and problems urinating, and later cysts, infections, infertility as well as complications in childbirth and increased risk of new-born deaths.
Emotional and Psychological Harm
Girls also experience emotional and psychological trauma as well as pain. Girls are likely to feel anger at the people who performed the FGM, arranged for it to be carried out and/or allowed it to happen. As these people will almost always be the girls' parents or close relatives, the girl will often experience profound feelings of betrayal and loss of trust.
After you're cut you're given presents, chocolates, sweets – me and my sister actually got gold watches. You're abused, but you're rewarded for it. It leaves you with a massive sense of confusion about people you trust [14].
(Leyla Hussain, anti-FGM campaigner)
Girls can experience post-traumatic stress disorder, with symptoms including flashbacks, anxiety and depression.
I only became aware of how much I'd been affected psychologically by female genital mutilation (FGM) when I fell pregnant. I was severely depressed and I hated being vaginally examined; it was my worst nightmare. And I remember the doctors wondering: why is she so scared? I realized later it was my body experiencing flashbacks, reminding me of what had happened to me when I was six.
(Leyla Hussain, anti-FGM campaigner)
5. Prevalence
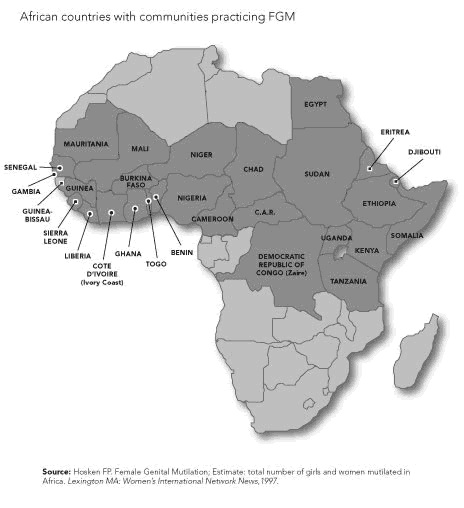
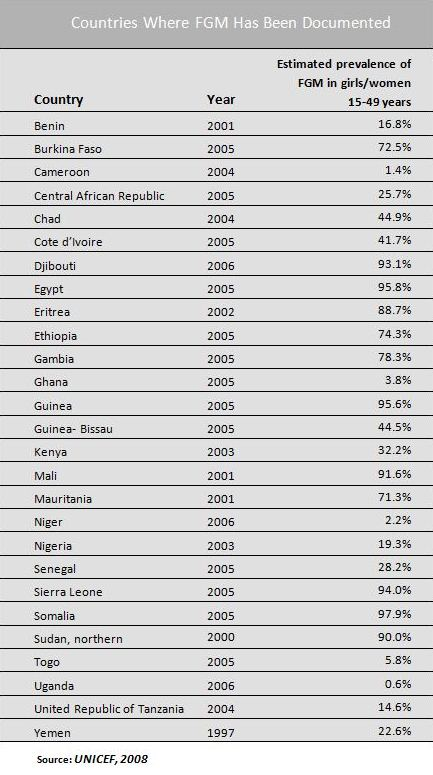
One or more types of FGM are practised in more than 28 African countries and also by ethnic groups in the southern part of the Arabian Peninsula and along the Persian Gulf. The World Health Organization (WHO) has also reported FGM has occurred in India, Indonesia, Iraq, Kurdistan, Israel, Malaysia and United Arab Emirates. There are also anecdotal reports FGM occurs in several other countries including Colombia, Democratic Republic of Congo, Oman, Peru and Sri Lanka
The WHO estimates that between 100 and 140 million girls and women worldwide have been subjected to one of the first three types of female genital mutilation. There are an estimated 3 million girls in Africa at risk of undergoing female genital mutilation every year.
The most common types of FGM are excision of the clitoris (Type 1), and excision of the clitoris and labia minora (Type 2) — accounting for up to 80% of all cases. The most extreme type is infibulation (Type 3), which constitutes about 15% of all procedures, but is practised among as many as 90% of women from Somalia, Djibouti and Northern Sudan — with a consequently higher rate of complications [15].
It should be noted that it is only the countries of Africa which currently collect data on FGM and hence maps and data tables can give the impression that it only takes place in Africa. In fact, by collecting data and acknowledging the issue, countries in Africa are providing a lead in the work to eradicate FGM.
[16] Taken from: fgm.co.nz/where-is-fgm-practiced
Mainly due to migration, women who have experienced FGM are increasingly found in the United Kingdom. Many women and girls will have experienced FGM before arrival in the UK and the number of women and girls from countries where FGM is practised is increasing:
- In 2011 an estimated 283,000 women aged 15-49 with FGM, born in countries in which it is practised, were living in England and Wales;
- This compares with the estimated 182,000 in 2001.
- Numbers of women born in the countries in the Horn of Africa [16], where FGM is almost universal and where the most severe Type III form, infibulation, is commonly practised, increased to 56,000 in 2011;
- The numbers of women from countries in East and West Africa, where FGM Types I and II also increased by 10,000 over the same period [17];
- See table below for a borough by borough breakdown of data of estimated numbers of girls born to women who have experienced FGM themselves.
Data on the numbers of girls at risk of FGM, or who have already experienced FGM is always estimated and largely based on prevalence studies in countries of origin. The impact of migration on prevalence is not currently known, however, it is important not to assume that prevalence will decease on migration – migration can encourage people to hold on to their traditions more strongly.
Estimated data is also now informed by data collected by health services in England on the number of girls and women who have had FGM. This data shows that from September 2014 – March 2015 [18]:
- 3,963 women were identified as having had FGM and 2,040 were from the London region;
- 60 cases of under 18s have been reported nationwide. The numbers are not broken down by region but, if it reflects the adult population, around 50% of these cases would be in London:
- In addition, as 77% cases of FGM come to the attention of health care professionals when women access maternity/obstetric services it is likely that the data under represents the number of girls who've had FGM;
- Finally, these numbers only reflect the girls and women who accessed health services within the 7 month period and hence represent a snap shot.
[16] That is Djibouti, Eritrea, Ethiopia, and Somalia
[17] This data is taken from, MacFarlane, A. and Dorkenoo, E. [2015] Prevalence of Female Genital Mutilation in England and Wales: National and local estimates.
[18] content.digital.nhs.uk/catalogue/PUB17463/fgm-mar-2015-exp-rep.pdf
6. Legislation and Statutory Guidance
FGM has been a criminal offence in the UK since 1985. In 2003 the Female Genital Mutilation Act was brought into legislation and under this act the practice of FGM carries a maximum prison term of 14 years for any UK national or permanent resident convicted of carrying it out, or aiding and abetting the process, while in the UK or overseas [19]. However, there has yet to be a single conviction.
The Serious Crime Act 2015 extended the offences relating to FGM to make parents or those responsible for caring for a child liable for failing to prevent their child being subjected to FGM. It also granted victims of FGM lifelong anonymity (the commencement date for these duties was 3 May 2015).
In addition, FGM civil protection orders (FGMPO) have been introduced in order to protect girls who are at risk of FGM or girls against whom a FGM offence has been committed. It also introduced a mandatory reporting duty requiring regulated health and social care professionals to report known cases of FGM in under 18s to the police.
FGM is a form of child abuse and violence against women and girls, and therefore should also be dealt with as part of existing child and adult protection structures, policies and procedures. The action we take to promote the welfare of children and protect them from harm is everyone's responsibility. Everyone who comes into contact with children and families has a role to play [20].
[19] www.legislation.gov.uk/ukpga/2003/31/contents
[20] www.gov.uk/government/publications/female-genital-mutilation-resource-pack/female-genital-mutilation-resource-pack
Mandatory Reporting
The Serious Crime Act 2015 introduced a legal duty for specific professional groups to report to the police any girl/ young woman who has had FGM (the Serious Crime Act 2015 inserted the duty into the FGM Act 2003). This duty applies when a girl informs the professional that FGM has been carried out on her and/or the professional observes physical signs on the girl appearing to show that FGM has been carried out. The duty applies to all teachers and all regulated health and social care professionals in England and Wales.
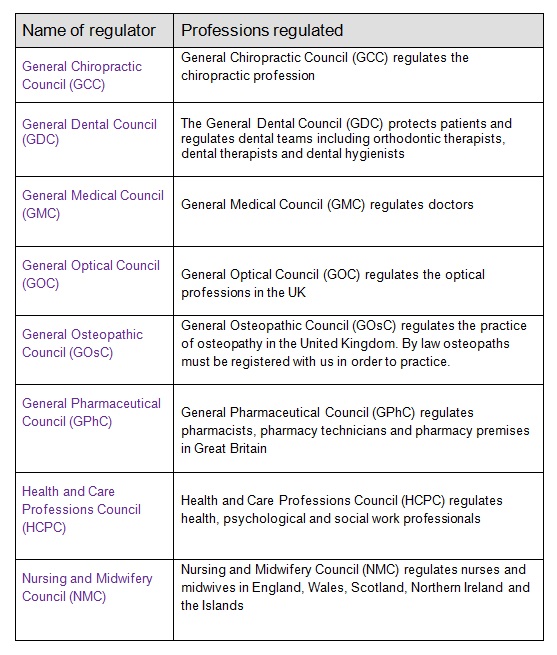
Regulated health and social care professionals include all professions regulated by a body overseen by the Professional Standards Authority. The PSA oversees the following regulatory bodies:
How to report
Where a professional, who is subject to the mandatory reporting duty, has either been told by a girl that she has had FGM or has observed a physical sign appearing to show that a girl has had FGM s/he should personally report the matter to the police by calling 101. Reports under the duty should be made as soon as possible after a case is discovered, and best practice is for reports to be made by the close of the next working day.
In all other cases, professionals should follow normal safeguarding processes and the Referral and Assessment Procedure. This is in line with guidance produced by NHS England and the Metropolitan Police Service.
For further information please refer to the recently published Home Office statutory guidance 'Mandatory Reporting of Female Genital Mutilation' and note 'Annex A – FGM mandatory reporting process map'.
Note the flow chart published by DH / NHSE 'FGM Mandatory reporting duty'.
7. Support for Victims
There is currently very little information available about what support services victims of FGM find beneficial, but the following should be taken into consideration when offering support:
- Girls may not know they have had FGM and may find it very difficult to come to terms with finding out;
- Girls may wish to have counselling and support in order to understand the implications for their sexual enjoyment and how to increase sexual pleasure;
- Victims can suffer post-traumatic stress disorder and require emotional and psychological support;
- Girls who come from practicing communities and do not go through FGM may experience rejection and intimidation from the community or families members. They may also fear their own sexuality and require support to understand the implications of not having experienced FGM;
- Girls who have experienced Type 3 FGM may wish to be de-infibulated;
- In some communities it is normal for women to be de-infibulated on marriage and in these circumstances women, some of whom may be under 18, may need support to understand issues of consent within marriage. Ideally these issues would also be discussed with the husband to be.
8. Risk Indicators
The primary risk factor for FGM is being a member of a practising community. See above section, 'Prevalence' for a list of countries where FGM is practiced. However, even in countries where prevalence is high there can be widely varying prevalence rates across different social and religious groups. Hence, when assessing risk it is always important to consider the particular circumstances and background of a child and her family.
In addition, it is the case that data on FGM is not collected in a number of countries where it is practiced (for example, Malaysia and Indonesia) and it is therefore important not to underestimate the risk girls from other countries may face.
Girls who are born to mothers or fathers who are not part of communities which practice FGM but have married into these communities or are otherwise very closely connected may also be at risk.
The most comprehensive risk assessment framework currently available is produced by the Department of Health – see Annex 1 of 'Female Genital Mutilation Risk and Safeguarding: Guidance for professionals (May 2016). The risk assessment is divided into the assessment of risk for children and adults.
Indicators which suggest an increased risk that a girl will experience, or has already experienced, FGM
- The girl's family comes from a community that practises FGM; and
- Members of a family, or the girl herself, say they support FGM.
- Members of a family appear ambivalent about FGM or refuse to discuss it.
NB It is important to ask families whether they intend to continue practicing FGM and ask girls (in age appropriate language) what they know about FGM and what their views are in relation to FGM. - She has female relatives who have had FGM.
This risk is likely to be heightened in the following circumstances:- It is known or believed likely to be the case that the FGM was carried out after migration from the country of origin;
- The female relative is within the close family network – including living with the girl;
- The female relative is herself a young woman and/or is close in age to the girl.
- She was born to a woman who has been subjected to FGM;
- This risk increases if a woman who has had type 3 FGM requests re-infibulation after giving birth as this suggests that either the woman herself believes in the importance of FGM or that her husband and/or family members require it of her.
Other risk indicators:
- The girl's family comes from a community that practises FGM and:
- She talks about a long holiday to her country of origin or another country where the practice is prevalent;
- She confides that she is to have a 'special procedure' or to attend a special occasion;
- She discloses concerns that she is at risk;
- She requests long or repeated toilet breaks from the classroom or spend long unexplained periods of time away from the classroom during the day – this may be the result of with bladder or menstrual problems if she has undergone Type 3 FGM;
- She has a prolonged absence from school with noticeable behaviour changes on her return;
- She is suffering from depression and/or self-harm or other mental health problems;
- Her parents/carers ask for her to be excused from physical exercise lessons without the support of her GP;
- Her parents/carers ask for her to be excused from sex education lessons;
- She is withdrawn from school without explanation or the explanation sounds implausible.
9. Roles and Responsibilities
Professionals and Volunteers in all Agencies
Professionals and volunteers working with children and young people need to be aware of which girls are at risk of experiencing FGM, be prepared to ask questions of those girls and their families regarding FGM and where necessary refer concerns to the police and children's social care for further investigation. All professionals and volunteers should also know the warning signs that FGM has taken place or may be about to take place and how to report these concerns.
Where a girl is thought to be at risk of FGM, practitioners should be alert to the need to act quickly - before FGM takes place. If any girl has symptoms or signs of FGM, or if there is good reason to suspect they are at risk of FGM, having considered their family history or other relevant factors, they must be referred to children's social care in line with Referral and Assessment Procedure. See also Referral and Assessment Procedure, Referral criteria.
Additionally, when a girl is identified as being at risk of FGM this information must be shared with the GP and, where the girl is under the age of 5, the health visitor should also be informed as part of the required safeguarding actions [21].
Where an adult woman is identified as having had FGM, enquiries should be made as to whether she has daughters or close female relatives under the age of 18. If she has, the risk that those girls have gone or may, in the future, undergo FGM should be assessed. Where there is insufficient information to adequately assess the risk a referral to children's social care should be considered. Where risk is identified a referral to children's social care should be made.
It is also critical that male partners, extended family members and boy children are not overlooked. Assessment of risk should include all family members as the views of male family members may be a protective factor or significantly increase the risk that FGM has been or will be carried out. Male family members will also require support and education.
[21] See the Child Protection s47 Enquiries Procedures
Mandatory Reporting
See above section on Mandatory Reporting. This is a legal duty, introduced by 'The Serious Crime Act 2015', that requires specific professional groups to report any known cases of FGM in under 18s which they identify in the course of their professional work to the police. Following consultation with social care professionals as well as other relevant professionals, only then will the police take action to ensure the girl/young woman is safe and her needs are prioritised.
'Known' cases are those where either a girl informs the person that an act of FGM – however described – has been carried out on her, or where the person observes physical signs on a girl appearing to show that an act of FGM has been carried out and the person has no reason to believe that the act was, or was part of, a surgical operation within section 1(2)(a) or (b) of the FGM Act 2003.
A failure to report the discovery in the course of their work could result in a referral to their professional body. The Home Office has produced guidance Mandatory Reporting of Female Genital Mutilation – procedural information to support this duty and a fact sheet on the new Duty for Health and Social Care Professionals and Teachers to Report Female Genital Mutilation (FGM) to the Police.
If there are suspicions that a girl under the age of 18 years may have undergone FGM or is at risk of FGM professionals must still report the issue by following their internal safeguarding procedures. Professionals must share the information about their concerns, potential risk and/or the actions which are to be taken. Next steps should be discussed with the safeguarding lead and where assessed as a concern a referral in line with the Referral and Assessment chapter should be made.
Health Services
Introduction
Female Genital Mutilation (FGM) is child abuse and the Department of Health and NHS England are committed to caring for FGM survivors, protecting girls from FGM, and preventing future generations from having to undergo FGM. However, despite this commitment and the fact that FGM has been illegal in the UK since 1985 and has always constituted child abuse, women and girls have not received the support and intervention they need.
But when it came to seeking medical support for her wounds, her experience of the NHS's FGM treatment was worlds apart from the newly implemented mandates. During each of her seven births, doctors failed to ask what had happened to her and merely wrote the acronym FGM on her files – made all the more galling by the fact she had never heard the term, and could barely speak English [22] (Hibo Wardere)
It is essential that FGM is not ignored – when health professionals identify that a woman has undergone FGM this should be always be discussed with the woman. Where a translator is required, it's important to ensure that they are independent of the woman and her family. It's also important that the woman understands any legal and medical terminology used. These discussions should address the ongoing physical, sexual and mental health needs of the woman as a result of FGM being carried out, as well as the risk to any children.
The Department of Health's Female Genital Mutilation Prevention Programme in partnership with NHS England has been launched and work on a range of FGM projects is now underway across NHS settings to improve the health response to FGM.
NHS Data Sharing
Female Genital Mutilation Information Sharing (FGM- IS) is a national IT system that supports the early intervention and ongoing safeguarding of girls, under the age of 18, who have a family history of Female Genital Mutilation (FGM).
FGM-IS is a service that supports the sharing of FGM information, and allows authorised healthcare professionals and administrative staff throughout England to view information about girls with a family history of FGM, regardless of care setting.
A national alert instigated by NHS Digital enables health professionals to add a ‘standard’ alert to a child’s summary care record (SCR) if it is highlighted they are at risk of FGM. The FGM-IS tab sits alongside the CP-IS (child protection information sharing) tab on the patient information page of their summary care record.
There are FGM risk assessments for safeguarding pregnant women/ a woman who has recently had a baby and children to help support decision making.
Identification and Risk Assessment
Health professionals in maternity services, GP surgeries and sexual health clinics are the most likely to encounter a girl or woman who has been subjected to FGM. Health professionals encountering a woman who has undergone FGM should be alert to the risk of FGM in relation to her:
- Younger siblings;
- Daughters or daughters she may have in the future;
- Extended family members.
When health professionals identify that the woman has or may have been mutilated they should carry out a risk assessment using, 'Annex 1 of 'Female Genital Mutilation Risk and Safeguarding: Guidance for professionals (May 2016)'.
It is critical that risk assessments are undertaken and that assessments are combined with supportive and educative work to assist women and their families to understand the legal framework and physical, sexual and psychological harm caused by FGM.
Health professionals should refer to CSC if their assessment raises concerns that a female child may have had, or be at risk of, FGM. They should also refer to CSC when they are unable to gather sufficient information to adequately assess the risk.
Re-infibulation
Where a woman who has had type 3 FGM has been de-infibulated in order to give birth she and her boyfriend / partner or husband must be told that re-infibulation is against the law and will not be done under any circumstances. Each woman should be offered counselling to address how things will be different for her afterwards.
After childbirth, a woman who has been de-infibulated may request and continue to request re-infibulation. This should be treated as a child protection concern, as the woman's apparent reluctance to comply with UK law and / or consider that the process is harmful raises concerns in relation to girl child/ren she may already have or may have in the future. Professionals should consult with their agency's designated safeguarding children professional and with local authority children's social care about making a referral to CSC.
Mandatory recording of FGM in a patient's healthcare record
Following publication of the Data Standard on 2nd April 2014, it became mandatory for any NHS healthcare professional to record within a patient's clinical record if they identify, through the delivery of healthcare services, that a woman or girl has had FGM.
For Acute Trusts from September 2014, it became mandatory to collate and submit basic anonymised details about the number of patients treated who have had FGM to the Department of Health every month. The first report of this anonymised data, reporting on the data from September, was published on 16th October and is available on the Health and Social Care Information Centre website.
There is no requirement to ask every girl and woman whether they have had FGM. The requirement is to record FGM in a patient's healthcare record only if and when it is identified during the delivery of any NHS healthcare. Professionals are reminded to be aware of the risk factors, including country of origin (see multi-agency guidelines for list of countries), and to use their professional judgement to decide when to ask the patient if they have had FGM.
It remains best practice to share information between healthcare professionals to support the on-going provision of care and efforts to safeguard women and girls against FGM. For example, after a woman has given birth, it is best practice to include information about her FGM status in the discharge summary record sent to the GP and Health Visitor, and to include that there is a family history of FGM within the Personal Girl Health Record (PCHR), often called the 'red book'.
Guidance for NHS professionals
Safeguarding women and girls at risk of FGM
This document provides practical help to support NHS organisations developing new safeguarding policies and procedures for female genital mutilation (FGM).
Commissioning services to support women and girls with FGM
This document sets out what some elements of a successful and safe service to support women and girls with female genital mutilation (FGM) might look like.
FGM eLearning
For more information please see E-Learning to Improve Awareness and Understanding of FGM.
Teachers and Nursery Workers
Teachers and nursery workers are key to the identification of girls who may be at risk and should therefore be aware of the risk factors for FGM and know how to report their concerns. They are often the only professionals who have ongoing relationships with girls and their families and are well placed to identify changes in the girls' behaviour or physical wellbeing. They might also be the only professionals who are aware that a girl from a practicing community is travelling to a country where FGM is practiced and that she may be at risk on this trip.
Nursery staff and some school staff might also change girls' nappies or clothes or assist girls to use the toilet and so they should have training to be alert to physical indicators that a girl/girl baby has had FGM and know how to report these concerns.
Nurseries and schools should also work with parents and carers to ensure they are:
- Aware that FGM is illegal in the UK;
- Aware of the harm associated with FGM;
- Support parents who do not wish their girls to have FGM.
It is important to emphasise that work with parents should include male members of the family as it is likely that they will be involved in any decisions as to whether a girl will have FGM or not.
Local Authorities
A referral to children's social care
On receipt of a referral, a decision should be made as to whether there is reasonable cause to suspect that a child is suffering, or is likely to suffer, significant harm. Where this is the case there should be a strategy meeting / discussion. See s47 thresholds and the multi-agency assessment.
Where the information at contact or referral does not identify risk in relation to FGM but nonetheless the information provided suggests there might be a risk, an assessment under section 17 of the Children's Act should be carried out.
Assessments should include the extended family and male members of the family as the decision to carry out FGM on a girl can be made and/or supported by different family members. Where families are likely to visit family members in countries where FGM is practiced, questions should also be asked about the views of those family members and of the communities in which they live. Families should be asked what plans they have made to keep their daughters safe on these visits and offered support around safety planning. This can include being given letters explaining the law to take with them when they go abroad.
All available family members should be informed that FGM is illegal and that this covers all types of FGM – it's been reported that the emphasis on the most severe forms of FGM can lead people to believe that other forms of FGM are not illegal.
There will be circumstances where it is decided that there isn't a risk of significant harm and no further action will be taken by children's social care. This might be the case where the information provided by the referrer is vague and non-specific – for example the only information provided is that a girl is believed to be from a community which practices FGM. The referrer might also have based their referral on incorrect information. In these circumstances, the referrer should be provided with the reasons why no further action is being taken.
Assessment of risk
The response to referrals of girls at risk of FGM should be proactive and must go beyond asking parents/carers if they intend to carry out FGM on their daughter. The assessment of those referrals should consider the risk indicators outlined in the above section. See also the Department of Health risk assessment, 'Annex 1 of 'Female Genital Mutilation Risk and Safeguarding: Guidance for professionals (May 2016)'.
Managing the medium and long term risk to a girl
Where it is decided that there is no known immediate risk to a girl but there is an ongoing risk that the girl will experience FGM as she grows to adulthood, prior to closing the case children's social care should ensure a plan is in place that addresses the following:
- Whole families have been informed of the law including explanations of the different types of FGM as there can be mistaken beliefs that some forms of FGM are not illegal;
- Families can be asked to sign a promise that they ensure their daughters do not undergo FGM;
- Flags can be put on passports alerting immigration staff to a girl who is at risk – the police can provide guidance;
- Victims of FGM can be allowed lifelong anonymity – including prohibiting the publication of any information that could lead to the identification of the victim. Publication covers all aspects of media including social media;
- The risk can be flagged on the girl's health records so that health services can continue to monitor the risk as the girl grows to adulthood;
- Universal services, particularly health, are informed of the concerns.
- Arrangements are made for these concerns to be passed on as a girl grows up. For example, as she moves from pre-school provision to primary and then secondary school;
- The plans should also ensure information about the risk will follow the girl if she moves address.
- Plans should also clarify for the relevant professionals in the girl's life, the risks that they should be alert to and the action they should take if they have further concerns.
Risk of significant harm
Where the assessment suggests that there is risk of significant harm, a strategy meeting/discussion must be convened within two working days and should involve representatives from the police, local authority children's social care, education, health and third sector services. Health providers or third sector organisations with specific expertise (e.g. FGM, domestic abuse and / or sexual abuse) must be invited, and consideration may also be given to inviting a legal advisor.
Outcome of strategy meeting/discussion
There are a number of different possible outcomes and these are summarised in Core Procedures. Available in the Child Protection s47 Enquiries Procedure.
It is important to note that if the strategy meeting / discussion decides that the girl is in immediate danger of mutilation then an emergency protection order should be sought.
If the girl has already undergone FGM, the police child abuse investigation team (CAIT) will take a lead role in the investigation.
Female Genital Mutilation Protection Orders
One outcome of a strategy meeting/discussion could be the decision to apply for an FGM Protection Order. Section 73 of the 2015 Serious Crime Act introduces FGM Protection Orders and local authorities can make an application to the family court for such an Order without first having to apply for the leave of the court to do so.
FGM Protection Orders (FGMPO) were introduced in order to protect victims or potential victims of female genital mutilation. The terms of and FGM Protection Order can be broad and flexible and enable the court to include whatever terms it considers necessary and appropriate to protect the girl. These include, for example, provisions requiring a person to surrender his or her passport [26]. Breach of an FGMPO is a criminal offence with a maximum penalty of five years' imprisonment, or as a civil breach punishable by up to two years' imprisonment.
Girls already known to children's social care
Where a girl comes from a practicing community and is being assessed by children's social care or is a 'child in need' or 'subject to a child protection' plan, there should be an assessment of the risk that she has experienced FGM or may do so in the future.
Children Looked After
Where a girl is looked after by children's social care and comes from a practicing community, children's social care should assess the risk that she has experienced FGM or may do so in the future.
Stepping down from children's social care
Where a girl at risk of FGM has been known to children's social care as a child in need, subject to a child protection plan or has been looked after, and the involvement of children's social care is coming to an end, the procedures outlined above in Managing the medium and long term risk should be followed. This applies even where the risk of FGM wasn't a reason for children's social care involvement but nonetheless this risk exists.
[25] www.legislation.gov.uk/uksi/2015/1422/pdfs/uksiem_20151422_en.pdf
[26] www.familylawweek.co.uk/site.aspx?i=ed145848
The Metropolitan Police Service
FGM is child abuse and any FGM investigation is dealt with by the Child Abuse Investigation Team (CAIT) in whose area the child permanently resides.
The priority for the police in any FGM investigation is prevention, protection, victim support and the prosecution of any offenders involved. This role should be undertaken in accordance with the principle of multi-agency co-operation to safeguard children.
Police may become aware of girls being victims of FGM or being at risk of FGM through the course of other criminal investigations, through referrals from the NSPCC FGM helpline and other agencies, or information direct from the public. The MPS is very keen to develop any intelligence opportunities in a recognised area of under-reported crime which therefore makes it difficult to detect. If there are any suspicions that a child is a victim of FGM or at risk of FGM, the police officer noting the concern should complete a Merlin report for referral to the multi-agency safeguarding hub (MASH), complete either a crime or a crime reported incident (CRI) on the MPS crime reporting information system (CRIS) and flag it PG to enable an appropriate action plan to be set. The matter will then be allocated to an appropriately trained officer to investigate from the appropriate Child Abuse Investigation Team. Police databases will be checked on every known family member and a risk assessment conducted.
The initial police response to information that a girl has had FGM or is at risk of FGM is to safeguard that child and prevent offences from happening. Where a girl is at immediate risk of being subjected to FGM, urgent action must be taken to remove them from the source of harm and ensure that any necessary evidence is secured. This action must be followed by referral to local authority's children's social care. A multi-agency strategy meeting will be convened. Consideration must also be given to other female siblings within the family or extended family who may also have had FGM or may be at risk of FGM.
In a Section 47 Children's Act investigation, every referral with regard to FGM must generate a multi-agency strategy meeting within 48 hours. FGM investigations must be investigated by a substantive Detective Constable. These officers will have received awareness training in FGM and the investigation will be subject to regular police supervisor reviews. The investigation will also be subject to regular ongoing multi-agency reviews to discuss the outcome and address any further protective steps that need to be taken with regard to the child and other siblings.
Where there are concerns that a girl may be at risk of FGM and the parents have been spoken to about the law, the dangers of FGM and adverse health implications but there is still a suggestion that the family intend to subject the child to FGM, the child must be protected. Officers should consider the use of Police Protection powers under Section 46 Children Act 1989 and remove her to a place of safety.
Referrals from local authority children's social care should be made direct to the local CAIT team. If the child is already known and has an assigned social worker, the referral will go to that social worker who will refer to the appropriate CAIT referral desk for creation of a CRIS report.
All interviews with the child as an actual or potential victim should be conducted, as far as possible, in accordance with the best evidence interview procedures. However, flexibility needs to be applied, as it may take a number of interviews before the child is able to make, or complete a statement/disclosure. Corroborative evidence must be sought through a medical examination conducted by a qualified paediatrician or doctor. The MPS has a memorandum of understanding with the FGM clinic at University College, London where specialists are willing to examine any girls under 18 where there is suspicion of FGM.
Where a child refuses to be interviewed or undergo medical examination, assistance must be sought from an intermediary or community organisation.
If the child has made a statement, victim support services should be considered as early as possible.
When made aware of cases of actual or suspected FGM, police should follow the Pan-London Operating Protocol for dealing with such cases. The MPS FGM toolkit sets out the corporate policy with regard to the investigation of allegations of FGM. The MPS has a memorandum of understanding with the CPS to enable early consultation to ensure that the best investigative strategies are adhered to in FGM investigations.
10. Local Safeguarding Children Partnerships
Local Safeguarding Children Partnerships (Local SCPs) should use available data on FGM prevalence to challenge the local multi agency partnership regarding the number of girls identified as having experienced FGM, the number of times agencies have intervened to protect girls and the number of prosecutions the following and whether these figures reflect what is known about the numbers of girls at risk. Data on the source of referral should also be collected in order to inform awareness raising and education and to hold agencies to account.
It is particularly important that Local SCPs ensure that they engage with local communities which practice FGM to ensure that the law in relation to FGM is understood, to encourage victims to come forward and seek help and to help change attitudes to FGM.
Appendix 1: Relevant Legislation
The Female Genital Mutilation Act 2003
Under the Female Genital Mutilation Act 2003 it is an offence in England, Wales and Northern Ireland for anyone (regardless of their nationality and residence status) to:
- Perform FGM in the UK;
- Assist the carrying out of FGM in the UK;
- Assist a girl to carry out FGM on herself in the UK; and
- Assist from the UK a non-UK person to carry out FGM outside the UK on a UK national or permanent UK resident.
It is also an offence for UK nationals or permanent UK residents to:
- Perform FGM on any person overseas;
- Assist FGM carried out abroad by a UK national or permanent UK resident – this would cover taking a girl abroad to be subjected to FGM;
- Assist a girl to perform FGM on herself outside the UK; and
- Assist FGM carried out abroad by a non UK person on a girl/woman who is a UK national or permanent UK resident – this would cover taking a girl abroad to be subjected to FGM;
Even in countries where the practice is not a criminal offence.
The Serious Crime Act 2015
In 2015 the legislative response to FGM was further strengthened through provisions in the Serious Crime Act 2015 (Part 5: Protection of children and others) See the Home Office factsheet.
- Section 70
Extend the reach of the extra-territorial offences in the 2003 Act to habitual (as well as permanent) UK residents;
Commencement 3 May 2015 - Section 71
Grant victims of FGM lifelong anonymity from the time an allegation is made; and
Commencement 3 May 2015 - Section 72
Make parents or those responsible for caring for a child liable for failing to prevent their child being subjected to FGM;
Commencement 3 May 2015 - Section 73
Create a new FGM civil protection order (FGMPO) to protect a girl who is at risk of FGM or a girl against whom a FGM offence has been committed.
Commencement 17th July 2015 - Section 74
Introduces a mandatory reporting duty requiring regulated health and social care professionals to report known cases of FGM in under 18s to the police.
Commencement 31st October 2015 - Section 75
Introduce guidance about female genital mutilation.
As above, the first three of these provisions came into force on 3 May 2015. The commencement dates for the FGMPO provisions and the mandatory reporting duty will be announced in due course.
Appendix 2: Guidance
Mandatory reporting of female genital mutilation: procedural information.
Safeguarding women and girls at risk of FGM (January 2017).
Includes the Department of Health risk assessment framework – see Annex 1 of 'Female Genital Mutilation Risk and Safeguarding: Guidance for professionals (May 2016). The risk assessment is divided into the assessment of risk for children and adults.
Additional guidance includes:


